Medical Equipments:
- Medication administration record (MAR)
- Prepared and labeled medication 50 ml solution bag from pharmacy
- Alcohol swab
- Secondary administration set
- Needle-less locking cannula
Nursing Procedures:
- Gather all of prepared equipments
- Wash your hand
- Check patient identification or arm-band
- Explain the procedures to the patient
- Observe the puncture site for redness and puffiness then palpate for tenderness
- Observe fluid infusing and check the patency of infusion site
- Remove IV container from the pole and lower the container below the level of infusion site
- Observe for backflow of blood into the hub of the venous access device and replace container on IV hole
- Secure the medication bag and check the prescription and the MAR
- Check patient's chart for allergies and drug compability
- Hang the secondary bag on IV hole
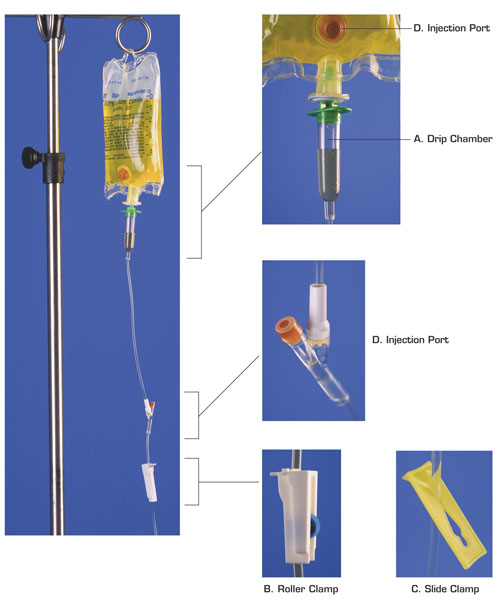
- Add the administration set to the secondary bag and prime the tubing
- Affix a needle-less locking cannula to the end of tubing
- Cleanse needle-less Y-site injection port of primary IV tubing closest to infusion site with an alcohol swab and allow to dry
- Insert needle-less locking cannula of secondary bag set into Y-site injection port of primary set ans secure in place with tape
- Affix the extension hook to the primary bag on the IV pole so that the primary bag hangs below the level of the secondary bag
- Open clamp of secondary tubing and adjust drip rate to desired infusion rate
- Observe patient for any signs or adverse reaction to the medication
- When secondary bag and drip chamber are empty, close the clamp on secondary system, readjust drip of primary solution as indicated and remove the secondary system
- Record medication infusion on the MAR and note any patient's responses














